What’s the purpose of the test?
The purpose is to do Investigation of fertility in Male.
Identify treatment options
Sample Collection
Methods of collection:-

Normal Semen analysis value as per World Health Organization (WHO)(WHO Manual for the Examination & Processing Of Human Semen (2010), Fifth Edition)
| Parameter | Lower reference limit |
| Semen volume (ml) | 1.5 (1.4 - 1.7) |
| Total sperms number (106 per ejaculate) | 37 (33 - 36) |
| Sperm Concentration (106 per ml) | 15 (12 - 16) |
| Total motility (PR + NP, %) | 40 (38 - 42) |
| Progressive motility (PR, %) | 32 (31 - 34) |
| Vitality (live spermatozoa, %) | 58 (55 - 63) |
| Sperm morphology (normal forms, %) | 4 (3.0 - 4.0) |
| Other consensus threshold values | |
| pH | >7.2 |
Note: PR - Progressive Motility, NP - Non Progressive Motility
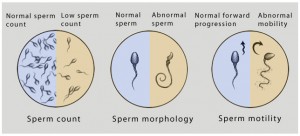
What's important in a semen analysis?
Many patients have had their initial fertility treatment decisions based on a semen analysis done at a regular medical reference lab. That's the same place that does your blood count, cholesterol and all the other medical tests that your general doctor orders. Their semen analysis consists of a check of semen volume, sperm concentration (count), motility (movement) and standard (WHO) morphology (an estimate of those normal shapes).
A Fertility specialist usually advises to get the semen analysis done at their own center by their Embryologist because the embryologist analyses the semen as per WHO standards and does a better analysis of sperm morphology which is an important parameter of semen analysis.
Importance of Sperm Morphology
The morphology of sperm is an important parameter to determine its fertilizing ability. The Egg (oocyte) is enclosed in a protein coat called as Zona Pellucida (ZP) through which the sperm has to pass/penetrate in order to fertilize the egg. If there is any defect in sperm morphology it will find it difficult to penetrate the ZP.
Abnormal Sperm shape: Abnormally shaped sperms often contain abnormal DNA i.e. it may have an extra chromosome or short of an chromosome or the DNA is packed in head in such a way that, if it at all it penetrates the ZP, the DNA would get all tangled up when it tries to form a chromosome inside the egg. Therefore the nature has evolved a way to keep abnormally shaped sperm from getting inside the egg and thereby maximizing the genetic development potential of the embryo.
“Sperm DNA Fragmentation Test can be performed to check the integrity of sperm DNA”
The difference is very important because we think that only perfectly shaped sperm are capable of fertilizing an egg.
There are three main causes of poor sperm morphology:
TERMS USED IN SEMEN ANALYSIS REPORT
Aspermia: absence of semen
Azoospermia: describes a total absence of spermatozoa in semen. (After centrifuge sperm count is zero/HPF).
Oligozoospermia: refers to a reduced number of spermatozoa in semen and is usually used to describe a sperm concentration of less than 15 million/ml. Sperm count 5-10 sperm/HPF.
Severe oligospermia: sperm count 1-2 sperm/HPF.
Polyzoospermia: denotes an increased number of spermatozoa in semen and is usually refers to a sperm concentration in excess of 350 million/ml.
Asthenozoospermia: refers to a man who produces a greater proportion of sperm which are immotile or have reduced motility, compared to the WHO reference values.
Teratozoospermia: sperm carry more morphological defects than usual
As a final note, sperm morphology scores can change a few percent from month to month and vary considerably amongst labs evaluating the same semen specimen. A single abnormal sperm morphology score is not conclusive. This is true for all seminal parameters. When the result of semen analysis is abnormal, the test should be repeated in 1-2 months to confirm the abnormality.
PCOS is a hormonal and Metabolic condition that affects women […]
04 Jun 22
IUI is a simple form of fertility treatment where motile […]
06 Aug 22
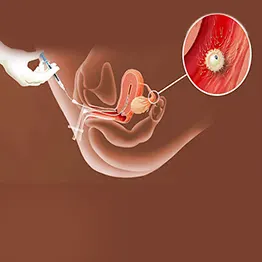
We are happy to have treated more than 20,000 couples with fertility issues. IUI is simple treatment for couples with unexplained Infertility, PCOS, early endometriosis Know More
Indicated in couples with tubal blockage, repeated failed IUI and endometriosis. Results range across 40 -50% at our centre Know More
Treatment of choice for male infertility with very low sperm count, obstructive azoospermia and for coupes requiring donor eggs. Know More
Many young men and women have utilized our fertility preservation services in the form of sperm, egg and embryo freezing either for medical or social reasons Know More

More than 3000 women have delivered at our centre. They have had an exceptional experience in antenatal care, delivery and postnatal care. Know More
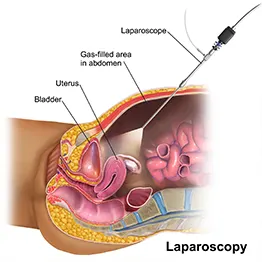
We have been performing all Gynaec surgeries through Laparoscopy for the past 25 years. Advantages are it is safe, less painful Know More
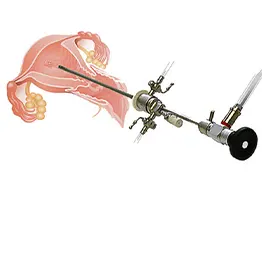
Hysteroscopy has many advantages over traditional D & C. We are equipped with small telescope to diagnose and treat pathologies inside the uterine cavity Know More
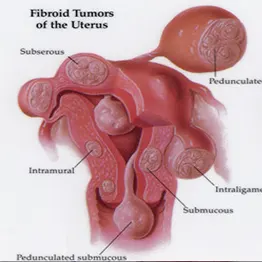
Fibroid causes infertility, pain and excessive menstrual blood loss. They can be operated through Laparoscopy or Hysteroscopy Know More
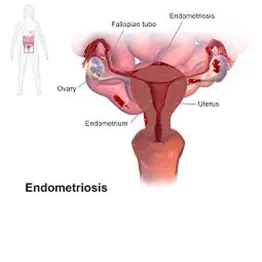
Endometriosis causes infertility and painful periods. Best treatment is initiated by Laparoscopy surgery and drugs Know More

We have been performing laparoscopic hysterectomy for the past 25 years. It is a definitive treatment for heavy menstrual bleeding, fibroids, cancer Know More
Ectopic is a condition where the pregnancy gets implanted in the fallopian tube instead of the uterine cavity. We have operated many cases laparoscopically Know More
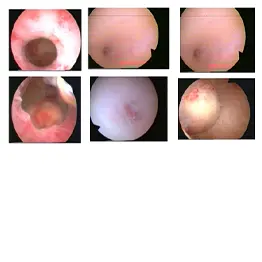
Hysteroscopy helps in evaluating the cause of Postmenopausal bleeding Know More

MD. DGO.,
Gynaec Endoscopy Surgeon Fertility and IVF Consultant

M.S. Obgy,
Fellowship in Reproductive Medicine and IVF (London), Minimal Access Surgery and Ultrasound

MS, DNB Obgy,
Fellowship in Reproductive Medicine and IVF (London), Minimal Access Surgery and Ultrasound
-Very satisfied.
-Doc Support indeed was very good .
-Nurse Support was absolutely Beneficial and excellent.
-Cleanliness was upto the mark.
-Hospitality made the stay comfortable.
KEEP IT UP!
Harshita Chhajed
We were so ecstatic on 9thapril 2022 as we hold our baby boy in our hands. We are so grateful as we were in the bestest and safest hands. All this was possible because of the talented doctors like you all-Dr Sudha Tandon, Dr Aditi Tandon, Dr Amrita Tandon and Dr Sachin. Dr Sudha Tandon and DrAditi Tandon helped us in our pregnancy journey by making themselves available all the time on phone. All our queries/questions were answered in no time which is by far the best response we could have received during covid times.
All doctors have given us bestest suggestions during our pregnancy journey in which we always had an utmost faith. It was a great time spent with you all during this pregnancy.
Thankyou so much for all the help/assistance/suggestions. We will always recommend Dr Tandon to our friends and relatives.
Sheela C Potdar
Dr Sudha Tandon and her two daughters make you feel comfortable and at ease. The flow of the process was smooth without making the patients wait unnecessarily.
Ashrita Katyal
Staff very polite and cordial.
Clean and neat hospital.
Cheerful ambience.
Doctor was very cooperative understanding and most importantaly non-judgemental. Made talking easier.
Thankyou for this wonderful offer and for making these tests accessible to all.
Odette Fred
-Staff very pleasant and polite.
-Dr too very polite.
-No waste of time.
-Clean place.
-Gives a good feel and not a nervous hospital feel.
Rosa Fred
Dr Sudha Tandon is one of the most oldest and the bestgynac in Chembur. Very good initative taken by them to keep a watch on the womenshealth on the occasion of the womensday.glad to see her daughters doing the job same as their mom.
All the best to both of them.
Thankyou
Satpal Bhambri
Thankyou for arranging this camp and providing services at affordable prices. The entire doctors team and also everyone right from the front desk staff to the staff nurses are really very cordial and soft-spoken.
My mother literally has a OBGY phobia :-o yet when she stepped out of the consulting room,she only told me they are all really great especially Dr AditiMaam.
Keep up the good work! I always recommend your name whenever any relatives/friends ask for a good OBGY in town.
Thankyou
Regards,
Dr Aditi Prabhu
Pratima Prabhu
-Very well organized.
-The staff is very competent.
-Quick process without any difficulties.
-Excellent time Management.
Kavita Bhatti
It is always reassuring to talk to Dr Sudha Tandon, Dr Amrita and Dr Aditi. It is for their expert advise and their compassionate approach that makes me come back to them for all my health related concives. I know I am in good hands.
Sheetal Patil
Thank you for this camp. Was done professionally and good staff.
Thanks again.
Kavita R.
Got to hear from a friend about this women’s day camp. Very well organized camp by Dr Sudha Tandon.
The price works well for all.
Thank-you
Mrs. Harvinder Saggi
I was absolutely satisfied with Doctor Amrita’s Consultation.
She cleared all my queries.
Thank you for having this women’s day camp.
Its really helpful.
Gunwant Saggi
My mother has also been Dr Sudha Aunty’s patient and it was but natural for me to follow same.I would like too extend my gratitude and thanks to Dr Sudha aunty for being there for me at every step.My sincere thanks to Dr Aditi and Dr Amrita who have always had my back and responded to every query and doubt with great promptness. Dr Aditi has been my “go-to-person” in times of anxiety.
A big thank you to all three of there for everything. I couldn’t have pulled this off without your support.
Dr Jayeeta Verma
What is infertility ?
If the couple has regular intercourse, does not use any contraception and still does not conceive within one year, they are said to be infertile. 80-85% of the couples conceive within one year of unprotected intercourse i.e. without the use of any contraceptive. However, the rest 15-20 % who are unable to conceive naturally are said to be infertile and these would require proper evaluation and help for getting pregnant.
Does fertility depend on age?
Yes, in a woman fertility does depend on her age. A young woman is naturally more fertile as she has more number of good quality eggs than a woman who is 35 +. Hence a woman who is 35 + should not wait for a long period for a natural conception and should seek help from a proper fertility expert. Also the chance of genetic abnormalities and medical complications like Hypertension and Diabetes increases with age.
When should a couple seek medical help for infertility?
If the woman is below 35 years and has normal menstrual periods, and the couple has tried for a conception for a year with a frequency of sexual intercourse 3-4 times a week during the fertile period and has yet not conceive, then they need to consult an Infertility expert.
How does body weight, diet & exercise affect fertility?
For increasing the chance of pregnancy, balanced body weight of the woman would be beneficial. Being obese or grossly underweight affects the maturation of eggs in the woman and hence may affect her fertility. Also, a grossly obese woman would have mechanical difficulty in having normal sexual relations. Regular, moderate exercise especially in the form of yogasanas, walking, swimming, or jogging prove beneficial for fertility. It has been observed that strenuous form of exercises for example jogging over 3 miles a day can hamper ovulation and hence may lead to decrease in fertility in the woman. Balanced and nutritious diet help increase the chances of conception and ensure proper growth of the fetus.
Is stress a major factor in infertility?
Chronic stress may interfere with the ovulation, may decrease the sexual desire and hence affect the frequency of sexual intercourse in the couple.
How would one know the cause of infertility?
A detailed history of both partners is very helpful in giving a clue to the cause of infertility. For e.g. anovulation is the cause of infertility in a woman who has irregular periods and who is also obese, blocked fallopian tubes in a woman with previous history of pelvic infection, low sperm count in a man with past history of mumps. Examination of both the partners, and getting the required investigations would give a complete picture.
What are the most stressful stages of IVF?
A natural conception is obviously what all couples desire and wish when they plan a pregnancy but when it does not happen and the couple is counselled for an IVF treatment, it creates lots of stress for them.
The most stressful part is the acceptance of the fact that IVF is the only best option for their problem. A good discussion with the doctor to understand about Human Reproduction and why IVF is the best option for them to conceive will help the couple .They should take their time to understand about what the treatment involves and always ask questions to get their doubts cleared. A session with the counsellor would definitely help. Speaking to friends and family who are knowledgeable is a good way to reduce the stress but at times it could be counterproductive especially if they only talk of the problems and are themselves not positive.
In an IVF treatment, the woman’s eggs and her partner‘s sperms are fertilised in a laboratory. To get her eggs, she needs to take hormonal Injections on a daily basis and at the same time every day. This could create some stress especially if she is in a demanding job. It is best that she confides in someone who is reliable and understands the intricacies of an IVF treatment. The best part is that these Injections are not painful as very fine needles are used and she could also self-administer it.
She needs to see her fertility specialist for the follicular tracking for about 4-5 times in a cycle. This could also be demanding and stressful. She should just take all this in her stride and not get unduly stressed. The follicular response may not be satisfactory especially in a woman with poor ovarian reserve and she could become stressed.
She could have stress on the day of egg retrieval because of the fear of pain but this is a small procedure which is done under safe anaesthesia. The procedure is done through the vagina and there are no cuts on her abdomen. This is simple and safe procedure, not painful. At times the male partner gets stressed and is unable to give his semen sample on the day of egg pickup. To avoid this problem, almost all fertility centres will freeze the semen sample beforehand as a backup.
Of course the other stressful point is to worry about the numbers and quality of eggs got at the time of pickup, the fertilization of the eggs, and the numbers of good quality embryos. All these are important form success point of view. A communication with the couple before the procedure will allay all their fears and will go a long way in taking care of the stress.
The most important step in IVF Treatment
The most important step in IVF is Embryo transfer for which the woman should relax. Generally it is done without anaesthesia. The woman‘s cooperation is so very important for favourable results.
After the embryo transfer one has to wait for about 10 days to know the results. It could be very stressful at this stage. She should try to be calm and not just keep thinking of the results. After the embryo transfer the woman has to use either progesterone vaginal tablets or Injections and the stress of finances adds to the stress of procedure.
All in all we do understand the stress that the couple undergoes for an IVF treatment cycle. Have trust in your doctor and you would definitely become a successful.
At our IVF Clinic in Mumbai and IVF centre in Navi Mumbai, we spend quite a lot of time to make you feel comfortable. Our entire support staff and our embryologist are in constant touch with the couple. We try to see that you do not have to wait for too long to see the doctor. We have all facilities of Hysteroscopy/ Laparoscopy / IVF treatment and Maternity at Dr Sudha Tandon centre and we take utmost care of our patients.